Impact of Pfizer's mRNA Vaccine on All-Cause Mortality: An Overview
Written on
Pfizer's six-month clinical trial of its mRNA Covid-19 vaccine revealed no significant differences in all-cause mortality rates between those who received the vaccine and those who received a placebo. Specifically, the trial reported 21 deaths in the vaccine group and 17 in the placebo group.

In theory, if vaccines are effective, the all-cause mortality rate should be lower in vaccinated individuals than in those who are unvaccinated. However, identical mortality rates could suggest that the vaccine has no life-saving effect, possibly due to ineffectiveness or adverse consequences. A higher mortality rate in the vaccinated group would raise concerns.
To summarize early, Pfizer's clinical trial did not demonstrate a reduction in all-cause mortality among those who received the mRNA vaccine. This may be attributed to a lack of high-risk participants in the study, making it less suitable for evaluating mortality outcomes. Other studies have shown different findings regarding Covid-19 vaccines and mortality rates.
Pfizer’s randomized controlled trial (RCT) indicated no net benefit in all-cause mortality when comparing the mRNA vaccine group to the placebo. According to their Biologics License Application (BLA) report submitted to the FDA in November 2021:
> “From Dose 1 [started on July 27, 2020] through the March 13, 2021 data cutoff date, there were a total of 38 deaths, 21 in the COMIRNATY [Pfizer’s mRNA vaccine] group and 17 in the placebo group. None of the deaths were considered related to vaccination.”
Thus, in the vaccine group of 21,047 participants, the mortality rate was approximately 0.0998%, while in the placebo group of 20,794 participants, it was around 0.0817%. This results in an absolute increase of roughly 0.02% and a relative increase of approximately 22%. However, the report did not assess whether this difference was statistically significant.
Statistical significance is defined as a p-value of less than 0.05, indicating that the observed difference is unlikely to have occurred by chance. I have reached out to experts to calculate the significance of the mortality rate in Pfizer's RCT, but have not received a response. Instead, I will provide a simple unadjusted rate ratio with a 95% confidence interval:
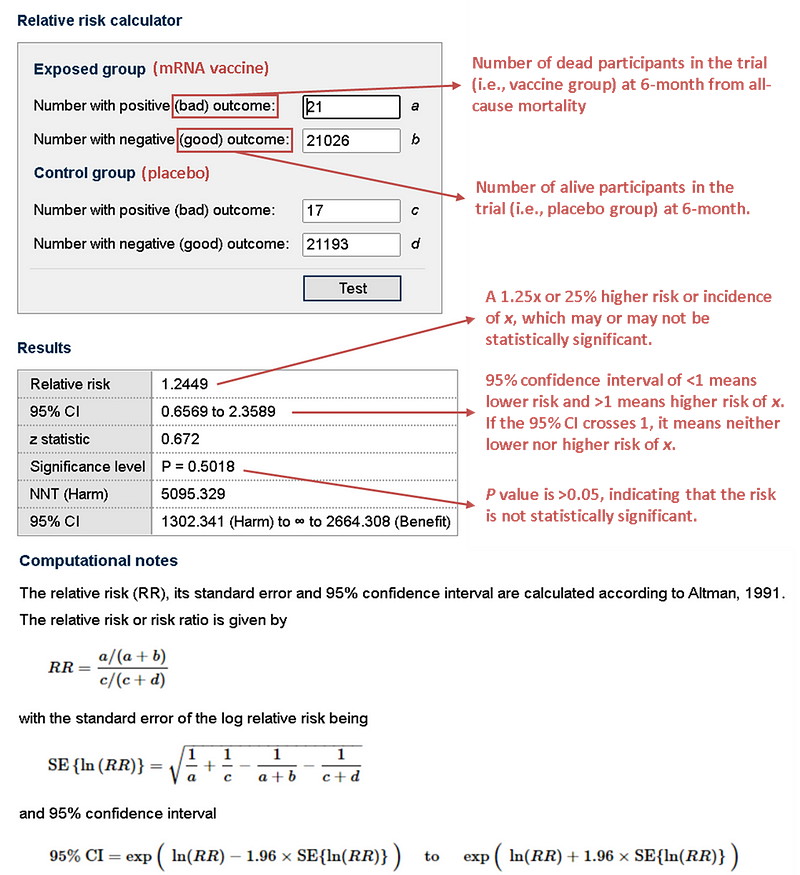
Calculating the unadjusted rate ratio indicates no statistically significant difference in mortality rates between the two groups, with a p-value of 0.5, which is well above the 0.05 threshold. Therefore, it is reasonable to conclude that the difference in deaths between the vaccine and placebo groups is attributable to random chance.
RCTs are designed to mitigate confounding variables such as age, gender, and pre-existing health conditions through randomization. Consequently, most RCTs provide unadjusted rate ratios, as randomization effectively controls for known and unknown confounders. This allows RCTs to establish causal relationships, unlike observational studies that are not randomized.
In terms of excess deaths, the vaccine group had four more deaths than the placebo group, translating to one additional death per 5,000 participants or 200 additional deaths per one million individuals. While these excess deaths raise concerns, they are not statistically significant.
Causes of Death in the Trial
A study published in the New England Journal of Medicine in November 2021 documented causes of death among participants in the Pfizer RCT:
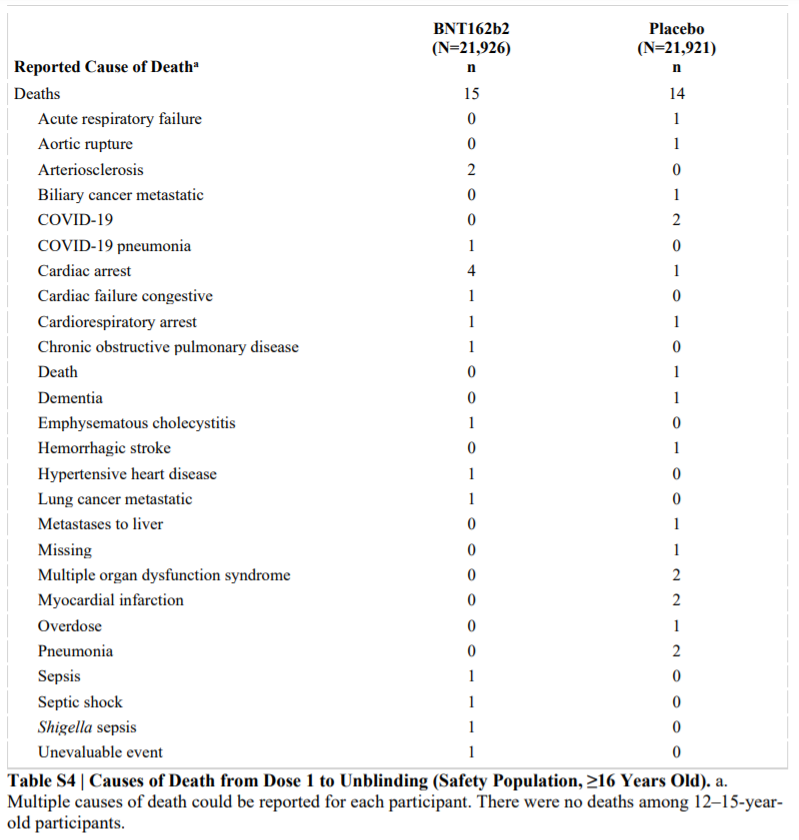
Initially, only 15 deaths in the vaccine group and 14 in the placebo group were reported. However, further analysis identified the totals as 21 and 17, respectively, as noted in the BLA report. Critics argue that Pfizer's disclosure regarding these deaths was insufficient, and they failed to demonstrate that the deaths were unrelated to the vaccine.
Excluding Covid-19 deaths, there were 20 non-Covid deaths in the vaccine group and 15 in the placebo group. Statistical analysis of these non-Covid deaths yielded a p-value of 0.39, indicating no significant difference in mortality risk.
Reasons for the Absence of Mortality Benefit
The Pfizer RCT primarily aimed to evaluate the efficacy of the mRNA vaccine in preventing symptomatic Covid-19, rather than fatal cases. Eligibility criteria included healthy individuals aged 16 and older, excluding immunocompromised individuals. Only a small percentage of participants were aged 75 or older, and only 21% had any pre-existing conditions. Furthermore, not all participants were exposed to the virus.
As a result, the study population lacked representation from those at higher risk of severe Covid-19, which could explain the absence of a mortality benefit.
During the trial, only one death from Covid-19 occurred in the vaccine group, compared to two in the placebo group. An increased number of high-risk participants might have led to a higher incidence of Covid-19 deaths in the placebo group, potentially revealing a mortality benefit associated with vaccination.
In essence, the Pfizer RCT was underpowered to detect significant differences in mortality rates, given the low fatality rate of Covid-19 among lower-risk groups. Dr. Tal Zaks from Moderna highlighted this limitation, stating that larger or longer studies would be required to observe rare outcomes.
Examining the causes of death across both groups, no single cause predominated, suggesting that if the vaccine were responsible for fatalities, we would expect a higher number of deaths attributed to a specific cause in the vaccine group. This may explain why trial investigators deemed these deaths non-vaccine-related.
Even when focusing on cardiac arrest, the most prevalent cause of death in the vaccine group, only four deaths occurred compared to one in the placebo group. The overall mortality differences were minimal, with unadjusted rate ratios showing no statistical significance.
Regardless of the all-cause mortality findings, the mRNA vaccines demonstrated efficacy in the RCT. They exhibited a 96% efficacy rate in preventing symptomatic Covid-19 shortly after the second dose, which decreased over time but remained effective against severe cases.
Insights from Other RCTs and Observational Studies
Further RCTs on Covid-19 vaccines have similarly indicated no statistically significant changes in all-cause mortality rates between vaccinated and placebo groups, as highlighted in a meta-analysis reviewing 35 trials. Notably, only one viral vectored DNA vaccine significantly reduced the risk of all-cause mortality by 73%.
However, it is essential to note that many of these trials had shorter follow-up durations compared to the comprehensive six-month Pfizer trial discussed earlier.
Observational studies have also been conducted regarding Covid-19 vaccines, but due to their non-randomized nature, they can only establish correlations rather than causation. Therefore, observational findings are best interpreted alongside RCT data.
A search in the PubMed database revealed 58 papers addressing all-cause mortality in relation to Covid-19 vaccination. Some notable studies include:
- Wilcox et al. (2021): Found that influenza vaccination was associated with a 24% lower odds of all-cause mortality among 6,921 individuals with Covid-19 in the UK.
- Baltas et al. (2021): Reported a 69% reduced risk of all-cause mortality among vaccinated Covid-19 cases compared to unvaccinated cases.
- Macchia et al. (2021): Indicated a 96% reduction in all-cause mortality among a large cohort in Argentina.
- Bardenheier et al. (2021): Suggested a 51% reduced risk of all-cause mortality in nursing home residents who received the vaccine.
- Xu et al. (2021): Found significant reductions in non-Covid mortality risk among vaccinated individuals in a large US cohort.
Despite the promising observational findings, the lack of randomization remains a critical limitation, leaving room for confounding factors. Additionally, there are issues with how vaccination status is defined, which could influence mortality classifications.
In conclusion, no observational studies to date have indicated that Covid-19 vaccines increase all-cause mortality. With consistent findings across various countries, we can be reasonably assured that Covid-19 vaccines do not elevate all-cause mortality rates at this time.
It is possible that the vaccines may not confer a mortality benefit, as suggested by Pfizer's trial results and other shorter-term studies. This could be attributed to a study population that is not at high risk for fatal Covid-19, or it may indicate that the vaccine is no longer effective against mortality. However, the least likely explanation for the equal mortality rates is that the vaccine causes harm equal to its benefits.
In summary, the six-month RCT of Pfizer's Covid-19 mRNA vaccine recorded 21 deaths in the vaccine group versus 17 in the placebo group, but this difference lacks statistical significance. Critics point out that the trial did not adequately address the potential link between these deaths and the vaccine. Despite the trial's conclusions, observational studies indicate a beneficial effect, supporting the notion that Covid-19 vaccines do not increase all-cause mortality rates.
If you've read this far, thank you! You can subscribe to my Medium email list for more insights. If you're interested in becoming a member for unlimited access to Medium, consider using my referral link, which provides me with a small commission at no extra cost to you. Any tips or support for my science writing efforts are greatly appreciated!